When the first vaccines for COVID-19 were being developed, I signed up to participate locally in the Moderna trial. My decision to roll up my sleeve and get the shot was based on two things: my familiarity with mRNA technology and my belief that mRNA technology is the future of vaccines long before the pandemic.
I understand some people’s hesitancy to get vaccinated. Is it safe? Will it work? How bad are the side effects? All good questions that are worth exploring.
Normally, for your body to develop neutralizing antibodies, you either have to get infected with the virus, or receive a vaccine. Historically, vaccines consist of a live attenuated virus (a virus that’s killed) or a little part of viral protein, so your body can develop antibodies to that virus or viral protein.
Historically, non-mRNA vaccines have taken a long time to develop. With mRNA technology, mRNA—the blueprint for making a critical piece of the virus—is injected into the body. The body makes that viral protein using the mRNA information and then makes antibodies specific to it.
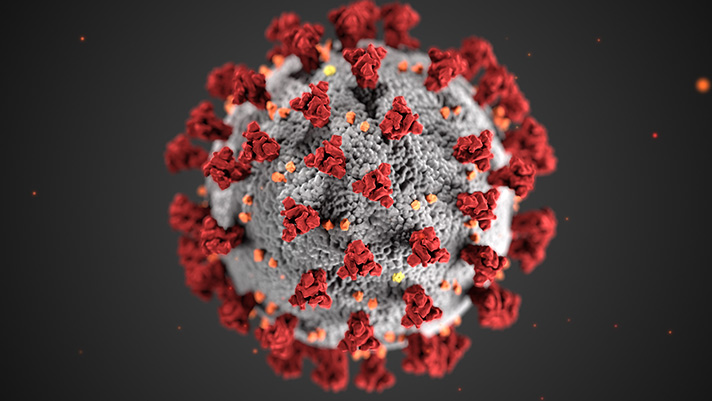
With COVID-19, the virus enters the body and attaches to a cell using its spike protein. This opens the door to allow all the virus’s information into the cell. The virus replicates in the cell and gets released into the body. After the infection has started, the body’s immune system kicks in to neutralize or kill the virus. The time from infection to replication to attacking the virus takes days. In the meantime, the body is getting crushed by infection.
With mRNA vaccines, a small portion of all the virus’s information is given. The body takes that information to produce a protein. The protein is recognized as a foreign adversary and the body attacks it. When the body sees that protein more than once, it reacts. That’s what happened when I got my second dose. I got a fever within six hours of vaccination that lasted about 12 hours. I felt pretty lousy for three days, then on the fourth day I woke up and felt fine.
The Pfizer and Moderna vaccines use mRNA technology. Both have been rigorously tested—about 70,000 patients in double-blind placebo-controlled trials—with very few adverse reactions. Total allergic reactions for both vaccines was lower than .02%. (For Pfizer, 11 people for every 1 million doses given had a reaction.)
In the United States, the fatality rate for a COVID-19 infection is around 1.7%. That’s about one to two people out of every 100 who get the infection. As bad as that is, the number doesn’t reflect other short- and long-term adverse effects such as blood clots, inflammation of the heart muscle and lung damage.
For me, getting vaccinated was a simple math problem. When I looked at the few adverse effects from vaccination versus the mortality rate and long-term adverse effects from a COVID-19 infection, it wasn’t even close. With vaccination, adverse effects are minimized and recovery is quicker. Getting vaccinated made sense.